Free Questions
Free MCQs in Surgery
Ameloblastoma
Q) Which of the following is true about ameloblastoma
a) It is seen in children below 5 years
b) It is the most common odontogenic tumor
c) Mandible is the most common site
d) It is highly malignant
Understanding Duodenal Atresia: Causes, Symptoms, and Treatment
Q) An infant presents with duodenal atresia. Which of the following is true about this condition?
a) It is the most common GI atresia
b) It presents soon after birth with non bilious vomiting
c) Pre natal detection of duodenal atresia is common
d) Gastro jejunostomy is the procedure of choice to bypass the obstruction
Understanding Duodenal Atresia in Infants: Key Facts and Diagnostic Insights
Duodenal atresia is a congenital condition that affects newborns, impacting their gastrointestinal (GI) system. While not the most common form of GI atresia, it is a significant condition that requires early detection and treatment. This article delves into the critical aspects of duodenal atresia, including its symptoms, diagnosis, and treatment options.
What is Duodenal Atresia?
Duodenal atresia is a congenital obstruction of the duodenum, the first part of the small intestine. This condition occurs in approximately 1 in 5,000 live births and is associated with other congenital malformations, such as Down syndrome, prematurity, and biliary atresia.
Prenatal Detection of Duodenal Atresia
Early Diagnosis through Ultrasound
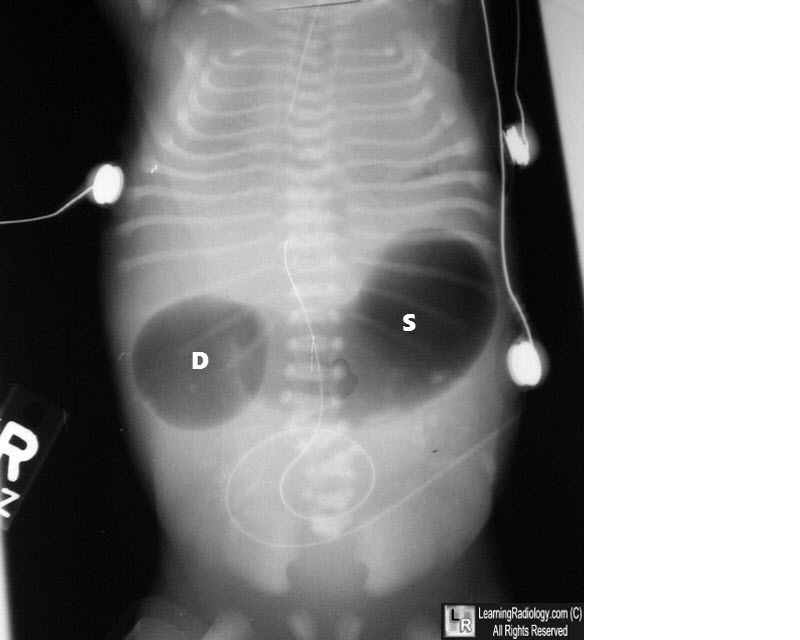
One of the most notable aspects of duodenal atresia is that it is commonly detected during prenatal ultrasounds. Advances in antenatal sonography allow doctors to identify most cases before birth, providing an opportunity for early planning and intervention. The typical sign on ultrasound is a "double bubble" appearance, which indicates the presence of fluid-filled areas in both the stomach and duodenum.
Symptoms and Presentation
Bilious Vomiting After Birth
Duodenal atresia typically presents soon after birth, with one of the hallmark symptoms being bilious vomiting. In around 80% of cases, the obstruction is located distal to the ampulla of Vater, allowing bile from the liver to mix with stomach contents, leading to greenish, bilious emesis.
Associated Congenital Conditions
Infants with duodenal atresia may also present with other congenital anomalies, such as Down syndrome, heart defects, or other gastrointestinal malformations like jejunoileal atresia, which is actually the most common type of GI atresia (occurring in 1 in 2,000 live births).
Types of Duodenal Obstructions
Stages of Duodenal Atresia
Duodenal atresia can occur in various forms, ranging from partial obstruction, such as duodenal webs, to complete separation of the duodenum. These different forms dictate the severity of symptoms and the urgency of intervention.
- Duodenal Webs – Thin membranes that partially block the duodenum.
- Stenosis – A narrowing of the duodenum that restricts food passage.
- Complete Atresia – A total obstruction where the duodenum is completely separated.
Diagnostic Features
Double Bubble Sign on Imaging
Postnatally, duodenal atresia is diagnosed through abdominal imaging, with the "double bubble" sign being a classic radiographic finding. This sign appears as two distinct gas-filled bubbles—one in the stomach and one in the duodenum—indicating the obstruction.
Treatment of Duodenal Atresia
Surgical Intervention
The treatment for duodenal atresia is surgical, with the goal of bypassing or removing the obstruction. Contrary to some misconceptions, gastrojejunostomy is not the preferred procedure. Instead, a duodenoduodenostomy is often performed to connect the two ends of the duodenum, allowing normal passage of food from the stomach to the intestines.
Post-Surgical Outlook
With early surgical intervention, the prognosis for infants with duodenal atresia is generally positive. Post-operative care is crucial to ensure proper digestion and prevent complications such as infection or malabsorption.
Bleeding Peptic ulcer
Q) In a 55 year old male with a bleeding peptic ulcer, endoscopy is done. Which of the following findings on endoscopy predicts the highest rate of re bleed?
a) Non bleeding vessel
b) Adherent clot
c) Flat pigmented spot
d) Clean base ulcer
Click here for more stomach MCQs
Free Answer
Answer a
a) Non bleeding vessel IIA - Out of the choices given
Bleeding peptic ulcer is mostly from the posterior surface of the lesion and can be sometimes lethal
Forrest classification is used to grade the risk of re bleeding in peptic ulcers.
According to the stigmata of recent bleed, the chances of re bleed increase.
Endoscopic appearance of bleeding peptic ulcer classification
Ia - Active Spurting Highest 90% chance of acute bleeding peptic ulcer ICD 10
Ib- Active oozing
IIa Non bleeding vessel 50% chance of re bleed
IIB Adherent clot
IIC Flat Pigmented spot
III Clean based ulcer
Sabiston 1154 21th edition
Q) How to treat a bleeding peptic ulcer? Bleeding gastric ulcer management?
Steps to manage a bleeding peptic ulcer
- Secure two large bore IV lines for fluid and blood products. Evaluate for coagulopathy
- Simultaneous evaluation for source of bleeding and history. Important causes to rule out are chronic liver disease, NSAID use etc
- Simultaneous IV PPI infusion
- Endoscopic control of bleeding peptic ulcer- Thermal coagulation, hemoclips, Adrenaline injections etc
- Operative procedure For Duodenum bleed - Longitudanally opening the anterior wall of duodenum and 3 point suture ligation
- For Gatric ulcer bleeding - depends on the site of ulcer and might require Antrectomy/Partial gastrectomy
Our Recommendations
BEST TEXTBOOKS FOR GENERAL SURGERY
Bailey & Love’s Short Practice of Surgery, 27th Edition
Sabiston’s Textbook of Surgery
Schwartz’s Principles Of Surgery
Contraindication of liver transplantation
Q)Contraindications of liver transplantation have changed over the years. Which is an absolute contraindication of liver transplantation
a) Previous breast cancer
b) Portal vein thrombosis
c) Active tuberculosis
d) Active substance abuse
Nutrient Absorption
Q) What is true regarding absorption of nutrients from small intestine?
a) Bile salt is required for absorption of Vitamin B12
b) Parathyroid hormone increases calcium absorption
c) Triglycerides are synthesized by intestinal epithelial cells before being released in portal circulation
d) Iron deficient individual can absorb 80% of dietary iron
Causes of Acalculus Cholecystitis
Q) Which of the following is not a cause of acalculus cholecystitis? Questions on bile duct
a) Kinking of the neck of gall bladder
b) Acalculus cholecystitis Sphincter spasm
c) Thrombosis of cystic artery
d) Over eating
Ans d
Acalculus cholecystitis can be both acute and chronic in the absence of stones. Although it can present acutely, acalculous cholecystitis typically presents more insidiously.
Mostly the acute form is recognized and chronic form is called biliary dyskinesia.
The cause of acalculus cholecystitis are
- Kinking or fibrosis of neck of gall bladder.
- Thrombosis of cystic artery
- Sphincter of Oddi spasm
- Prolonged fasting
- Dehydration
- Sepsis
- Systemic diseases MODS
Jaundice in acalculus cholecystitis is known to occur because of ischemia and inflammation cystic duct gets obstructed due to edema
Diagnosis
Chronic acalculus cholecystitis is a cholescintigraphy nuclear scan (HIDA) with the administration of cholecystokinin (CCK). After the . A calculated ejection fraction of 35% or less may be indicative of hypokinetic functioning of the gallbladder. An ultrasound of the gallbladder may also be useful. If this shows a thickened gallbladder wall of over 3.5 mm, this may be due to cholecystitis.
Acute acalculus cholecystitis - USG CT or HIDA
BEST BOOKSMCQ practise
MRCS Part A: Essential Revision Notes: Book 2
Omental cyst
Q) True statement about omental cyst is ?
a) It is always unilocular
b) Commonly seen in old age group
c) Arise from acquired or congenital obstruction of the lymphtaic channels
d) Complications are more common in old age.
Answer c
Lymph node stations in Carcinoma stomach
Q) In gastric cancer, lymph node station 12 corresponds to
a) Common hepatic
b) Hepatoduodenal
c) Retropancreatic
d) Superior Mesenteric
Altemeier procedure
Q) True about altemeier procedure?
a) It is proctosigmoidectomy with posterior levataroplasty
b) Done in left lateral position
c) Recurrence rate can be as high as 50%
d) Altemeier was the 1st person to do it